Shigella(lat. Shigella) is a genus of gram-negative, facultative anaerobic bacteria that are causative agents of dysentery.
Shigella in the taxonomy of bacteria
Shigella genus (lat. Shigella) is part of the Enterobacteriaceae family (lat. Enterobacteriaceae), order Enterobacteriaceae (lat. Enterobacteriales), class Gammaproteobacteria (lat. γ proteobacteria), type of proteobacteria (lat. Proteobacteria), kingdom of bacteria.The Shigella genus includes 4 species corresponding to four serogroups:
- shigella dysentery ( Shigella dysenteriae), serogroup A, includes 12 serotypes
- shigella flexnera ( Shigella flexneri), serogroup B - 6 serotypes
- shigella boyd ( Shigella boydii), serogroup C - 23 serotypes
- shigella sonne ( Shigella sonnei), serogroup D - 1 serotype
Shigella. General information
Shigella have the appearance of rods without flagella, with rounded ends measuring 2-3 by 0.5-0.7 microns. They do not form spores or capsules. Shigella is poorly resistant to physical, chemical and biological environmental factors. Shigella lives in water, soil, food, on objects, dishes, vegetables, and fruits for 5–14 days. At a temperature of 60 °C, Shigella die in 10–20 minutes, at 100 °C - instantly. Direct sunlight kills Shigella within 30 minutes. In the absence of sunlight, high humidity and moderate temperatures, Shigella remains viable in the soil for up to 3 months. Shigella can survive in gastric juice for only a few minutes. In stool samples, Shigella die from the acidic reaction of the environment and antagonist bacteria after 6–10 hours. In dried or frozen stool, Shigella is viable for several months.
Direct sunlight kills Shigella within 30 minutes. In the absence of sunlight, high humidity and moderate temperatures, Shigella remains viable in the soil for up to 3 months. Shigella can survive in gastric juice for only a few minutes. In stool samples, Shigella die from the acidic reaction of the environment and antagonist bacteria after 6–10 hours. In dried or frozen stool, Shigella is viable for several months. The most resistant to external influences is the Shigella species Shigella sonnei, least stable - Shigella dysenteriae.
Infection occurs through the fecal-oral or household contact route, through water and food products. Shigellosis can be transmitted by flies and cockroaches.
Shigellosis is characterized by constant dull pain throughout the abdomen, which later becomes acute cramping, localized in the lower abdomen, usually on the left or above the pubis. During the act of defecation, nagging pain in the rectal area, radiating to the sacrum. Initially, frequent bowel movements - up to 10–25 per day, mainly from mucus with inclusions of blood, and in a later period, admixtures of pus. False urge to defecate - tenesmus - is frequent.
 Bacterial dysentery (shigellosis) has an incubation period from several hours to 7 days, most often occurs acutely and is manifested by malaise, chills, headache, fever, convulsions, single or repeated vomiting. The patient's temperature rises. At the same time or slightly later, abdominal pain appears. Full recovery occurs in 2–3 weeks. In some patients, dysentery becomes chronic.
Bacterial dysentery (shigellosis) has an incubation period from several hours to 7 days, most often occurs acutely and is manifested by malaise, chills, headache, fever, convulsions, single or repeated vomiting. The patient's temperature rises. At the same time or slightly later, abdominal pain appears. Full recovery occurs in 2–3 weeks. In some patients, dysentery becomes chronic.
In the United States, Shigella is the third (after Salmonella and Campylobacter) cause of foodborne illnesses and hospitalizations. In 2010, there were a total of 1,780 cases of shigellosis reported in the United States. 333 sick people were hospitalized. However, fatal shigellosis, unlike a number of other food infections, has not been recorded.
See also: American College of Gastroenterology Tips for Food Poisoning (translation into Russian of a release published in the USA on June 3, 2011 in connection with the infection in Europe).
Treatment of dysentery caused by shigella
For the treatment of shigella dysentery, WHO recommends (“Treatment of diarrhea.” 2006):- as the antibiotic of choice - ciprofloxacin 500 mg twice a day for adults, 15 mg per kg of body weight twice a day for children, taken for three days
- as alternative antibacterial agents:
- pivmecillin 400 mg 4 times a day for adults, 20 mg per kg of body weight twice a day for children, taken for five days or
- ceftriaxone - in children 50-100 mg per kg of body weight intramuscularly for 2-5 days
- When choosing an antibiotic, take into account the results of drug sensitivity studies of strains Shigella, isolated recently in a specific area.
Antibiotics active against Shigella
Antibacterial agents (those described in this reference book) active against Shigella:Microbiology of dysentery
Dysentery is an infectious disease characterized by general intoxication of the body, diarrhea and a peculiar lesion of the mucous membrane of the large intestine. It is one of the most common acute intestinal diseases in the world. The disease has been known since ancient times under the name “bloody diarrhea”, but its nature turned out to be different. In 1875, the Russian scientist F.A. Lesh isolated an amoeba from a patient with bloody diarrhea Entamoeba histolytica, in the next 15 years, the independence of this disease was established, for which the name amoebiasis was retained.
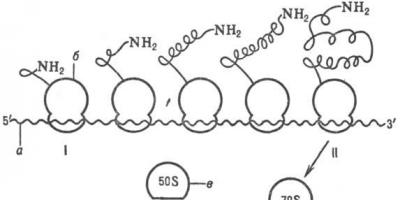
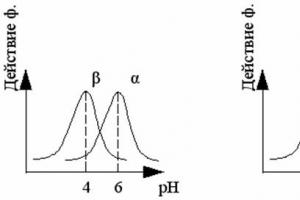
The causative agents of dysentery proper are a large group of biologically similar bacteria, united in the genus Shigella. The pathogen was first discovered in 1888 by A. Chantemes and F. Vidal; in 1891 it was described by A.V. Grigoriev, and in 1898 K. Shiga, using serum obtained from a patient, identified the pathogen in 34 patients with dysentery, finally proving the etiological role of this bacterium. However, in subsequent years, other causative agents of dysentery were discovered: in 1900 - by S. Flexner, in 1915 - by K. Sonne, in 1917 - by K. Stutzer and K. Schmitz, in 1932 - by J. Boyd , in 1934 - D. Large, in 1943 - A. Sax. Currently genus Shigella includes more than 40 serotypes. All of them are short, non-motile gram-negative rods that do not form spores or capsules, which grow well on regular nutrient media and do not grow on starvation media with citrate or malonate as the sole carbon source; do not form H 2 S, do not have urease; the Voges–Proskauer reaction is negative; glucose and some other carbohydrates are fermented to form acid without gas (except for some biotypes Shigella flexneri: S. manchester And S. newcastle); As a rule, they do not ferment lactose (with the exception of Shigella Sonne), adonitol, salicin and inositol, do not liquefy gelatin, usually form catalase, and do not have lysine decarboxylase and phenylalanine deaminase. The content of G + C in DNA is 49 – 53 mol%. Shigella are facultative anaerobes, the optimum temperature for growth is 37 °C, they do not grow at temperatures above 45 °C, the optimal pH of the environment is 6.7 - 7.2. Colonies on dense media are round, convex, translucent; in case of dissociation, rough R-form colonies are formed. Growth on MPB in the form of uniform turbidity, rough forms form a sediment. Freshly isolated cultures of Shigella Sonne usually form colonies of two types: small round convex (phase I), large flat (phase II). The nature of the colony depends on the presence (phase I) or absence (phase II) of a plasmid with a molecular weight of 120 MD, which also determines the virulence of Shigella Sonne.
The international classification of Shigella is based on their biochemical characteristics (mannitol-non-fermenting, mannitol-fermenting, slowly lactose-fermenting Shigella) and features of the antigenic structure (Table 37).
In Shigella, O-antigens of different specificity were found: common to the family Enterobacteriaceae, generic, species, group and type-specific, as well as K-antigens; They do not have N-antigens.
Table 37
Classification of bacteria genus Shigella
The classification takes into account only group and type-specific O-antigens. In accordance with these characteristics, the genus Shigella is divided into 4 subgroups, or 4 species, and includes 44 serotypes. In subgroup A (type Shigella dysenteriae) included Shigella, which does not ferment mannitol. The species includes 12 serotypes (1 – 12). Each serotype has its own specific type antigen; antigenic connections between serotypes, as well as with other Shigella species, are weakly expressed. To subgroup B (type Shigella flexneri) include Shigella, which usually ferments mannitol. Shigella of this species are serologically related to each other: they contain type-specific antigens (I – VI), by which they are divided into serotypes (1 – 6), and group antigens, which are found in different compositions in each serotype and by which the serotypes are divided into subserotypes. In addition, this species includes two antigenic variants - X and Y, which do not have typical antigens; they differ in sets of group antigens. Serotype S. flexneri 6 has no subserotypes, but it is divided into 3 biochemical types according to the characteristics of the fermentation of glucose, mannitol and dulcitol (Table 38).
Table 38
Biotypes S. flexneri 6

Note. K – fermentation with the formation of only acid; CG – fermentation with the formation of acid and gas; (–) – no fermentation.
Lipopolysaccharide antigen O in all Shigella Flexner contains group antigen 3, 4 as the main primary structure, its synthesis is controlled by a chromosomal gene localized near the his-locus. Type-specific antigens I, II, IV, V and group antigens 6, 7, 8 are the result of modification of antigens 3, 4 (glycosylation or acetylation) and are determined by the genes of the corresponding converting prophages, the site of integration of which is located in the lac - pro region of the Shigella chromosome.
Appeared in the country in the 80s. XX century and a new subserotype that has become widespread S. flexneri 4(IV:7, 8) differs from subserotype 4a (IV:3, 4) and 4b (IV:3, 4, 6), arose from a variant S. flexneri Y(IV:3, 4) due to lysogenization by its converting prophages IV and 7, 8.
To subgroup C (type Shigella boydii) include Shigella, which usually ferments mannitol. Members of the group are serologically different from each other. Antigenic connections within the species are weakly expressed. The species includes 18 serotypes (1 – 18), each of which has its own main type antigen.
In subgroup D (type Shigella sonnei) included Shigella, which usually ferment mannitol and are capable of slowly (after 24 hours of incubation and later) fermenting lactose and sucrose. View S. sonnei includes one serotype, but colonies of phases I and II have their own type-specific antigens. For the intraspecific classification of Shigella Sonne, two methods have been proposed:
1) dividing them into 14 biochemical types and subtypes according to their ability to ferment maltose, rhamnose and xylose; 2) division into phage types according to sensitivity to a set of corresponding phages.
These typing methods have mainly epidemiological significance. In addition, Shigella Sonne and Shigella Flexner are typed for the same purpose based on their ability to synthesize specific colicins (colicinogenotyping) and sensitivity to known colicins (colicinotyping). To determine the type of colicins produced by Shigella, J. Abbott and R. Chenon proposed sets of standard and indicator strains of Shigella, and to determine the sensitivity of Shigella to known types of colicins, a set of standard colicinogenic strains of P. Frederick is used.
Resistance. Shigella has a fairly high resistance to environmental factors. They survive on cotton fabric and paper for up to 30 - 36 days, in dried feces - up to 4 - 5 months, in soil - up to 3 - 4 months, in water - from 0.5 to 3 months, on fruits and in vegetables – up to 2 weeks, in milk and dairy products – up to several weeks; at a temperature of 60 °C they die in 15 – 20 minutes. Sensitive to chloramine solutions, active chlorine and other disinfectants.
Pathogenicity factors. The most important biological property of Shigella, which determines their pathogenicity, is the ability to invade epithelial cells, multiply in them and cause their death. This effect can be detected using a keratoconjunctival test (introducing one loop of a Shigella culture (2–3 billion bacteria) under the lower eyelid of a guinea pig causes the development of serous-purulent keratoconjunctivitis), as well as by infecting cell cultures (cytotoxic effect) or chicken embryos (their death) , or intranasally in white mice (development of pneumonia). The main pathogenicity factors of Shigella can be divided into three groups:
1) factors determining interaction with the epithelium of the mucous membrane;
2) factors that ensure resistance to humoral and cellular defense mechanisms of the macroorganism and the ability of Shigella to reproduce in its cells;
3) the ability to produce toxins and toxic products that determine the development of the pathological process itself.
The first group includes adhesion and colonization factors: their role is played by pili, outer membrane proteins and LPS. Adhesion and colonization are promoted by enzymes that destroy mucus - neuraminidase, hyaluronidase, mucinase. The second group includes invasion factors that promote the penetration of Shigella into enterocytes and their reproduction in them and in macrophages with the simultaneous manifestation of a cytotoxic and (or) enterotoxic effect. These properties are controlled by the genes of a plasmid with a molecular weight of 140 MD (it encodes the synthesis of outer membrane proteins that cause invasion) and the chromosomal genes of Shigella: kcp A (causes keratoconjunctivitis), cyt (responsible for cell destruction), as well as other genes not yet identified. Protection of Shigella from phagocytosis is provided by the surface K-antigen, antigens 3, 4 and lipopolysaccharide. In addition, lipid A of Shigella endotoxin has an immunosuppressive effect: it suppresses the activity of immune memory cells.
The third group of pathogenicity factors includes endotoxin and two types of exotoxins found in Shigella - Shiga and Shiga-like exotoxins (SLT-I and SLT-II), the cytotoxic properties of which are most pronounced in S. dysenteriae 1. Shiga and Shiga-like toxins have also been found in other serotypes S. dysenteriae, they are also formed S. flexneri, S. sonnei, S. boydii, EHEC and some salmonella. The synthesis of these toxins is controlled by the tox genes of converting phages. Type LT enterotoxins are found in Shigella Flexner, Sonne and Boyd. Their LT synthesis is controlled by plasmid genes. Enterotoxin stimulates the activity of adenylate cyclase and is responsible for the development of diarrhea. Shiga toxin, or neurotoxin, does not react with the adenylate cyclase system, but has a direct cytotoxic effect. Shiga and Shiga-like toxins (SLT-I and SLT-II) have a molecular weight of 70 kDa and consist of subunits A and B (the latter of 5 identical small subunits). The receptor for toxins is a glycolipid of the cell membrane.
The virulence of Shigella Sonne also depends on a plasmid with a molecular weight of 120 MD. It controls the synthesis of about 40 outer membrane polypeptides, seven of them are associated with virulence. Shigella Sonne, having this plasmid, form phase I colonies and are virulent. Cultures that have lost the plasmid form phase II colonies and lack virulence. Plasmids with a molecular weight of 120–140 MD were found in Shigella Flexner and Boyd. Shigella lipopolysaccharide is a strong endotoxin.
Features of epidemiology. The source of infection is only humans. No animals in nature suffer from dysentery. Under experimental conditions, dysentery can only be reproduced in monkeys. The method of infection is fecal-oral. Routes of transmission: water (predominant for Shigella Flexner), food, especially milk and dairy products (predominant route of infection for Shigella Sonne), and household contact, especially for the species S. dysenteriae.
A feature of the epidemiology of dysentery is a change in the species composition of pathogens, as well as Sonne biotypes and Flexner serotypes in certain regions. For example, until the end of the 30s. XX century to a share S. dysenteriae 1 accounted for up to 30–40% of all cases of dysentery, and then this serotype began to occur less and less often and almost disappeared. However, in the 1960s - 1980s. S. dysenteriae reappeared on the historical arena and caused a series of epidemics that led to the formation of three hyperendemic foci of it - in Central America, Central Africa and South Asia (India, Pakistan, Bangladesh and other countries). The reasons for the change in the species composition of dysentery pathogens are probably associated with changes in collective immunity and changes in the properties of dysentery bacteria. In particular, the return S. dysenteriae 1 and its widespread distribution, which caused the formation of hyperendemic foci of dysentery, is associated with its acquisition of plasmids that caused multidrug resistance and increased virulence.
Features of pathogenesis and clinic. The incubation period for dysentery is 2–5 days, sometimes less than a day. The formation of an infectious focus in the mucous membrane of the descending part of the large intestine (sigmoid and rectum), where the dysentery pathogen penetrates, is cyclical in nature: adhesion, colonization, introduction of Shigella into the cytoplasm of enterocytes, their intracellular reproduction, destruction and rejection of epithelial cells, release of pathogens into the lumen intestines; after this, the next cycle begins - adhesion, colonization, etc. The intensity of the cycles depends on the concentration of pathogens in the parietal layer of the mucous membrane. As a result of repeated cycles, the inflammatory focus grows, the resulting ulcers, connecting, increase the exposure of the intestinal wall, as a result of which blood, mucopurulent lumps, and polymorphonuclear leukocytes appear in the feces. Cytotoxins (SLT-I and SLT-II) cause cell destruction, enterotoxin – diarrhea, endotoxins – general intoxication. The clinical picture of dysentery is largely determined by what type of exotoxin is produced to a greater extent by the pathogen, the degree of its allergenic effect and the immune status of the body. However, many questions of the pathogenesis of dysentery remain unclear, in particular: the features of the course of dysentery in children of the first two years of life, the reasons for the transition of acute dysentery to chronic, the significance of sensitization, the mechanism of local immunity of the intestinal mucosa, etc. The most typical clinical manifestations of dysentery are diarrhea, frequent urge: in severe cases, up to 50 or more times a day, tenesmus (painful spasms of the rectum) and general intoxication. The nature of the stool is determined by the degree of damage to the large intestine. The most severe dysentery is caused by S. dysenteriae 1, most easily - Sonne dysentery.
Post-infectious immunity. As observations of monkeys have shown, after suffering from dysentery, strong and fairly long-lasting immunity remains. It is caused by antimicrobial antibodies, antitoxins, increased activity of macrophages and T-lymphocytes. Local immunity of the intestinal mucosa, mediated by IgAs, plays a significant role. However, immunity is type-specific; strong cross-immunity does not occur.
Laboratory diagnostics. The main method is bacteriological. The material for research is feces. Pathogen isolation scheme: inoculation on differential diagnostic media Endo and Ploskirev (in parallel on enrichment medium followed by inoculation on Endo and Ploskirev media) to isolate isolated colonies, obtaining a pure culture, studying its biochemical properties and, taking into account the latter, identification using polyvalent and monovalent diagnostic agglutinating sera. The following commercial serums are produced.
1. To Shigella, which does not ferment mannitol:
To S. dysenteriae 1 And 2
To S. dysenteriae 3 – 7(polyvalent and monovalent),
To S. dysenteriae 8 – 12(polyvalent and monovalent).
2. To Shigella fermenting mannitol:
to typical antigens S. flexneri I, II, III, IV, V, VI,
to group antigens S. flexneri 3, 4, 6, 7, 8– polyvalent,
to antigens S. boydii 1 – 18(polyvalent and monovalent), to antigens S. sonnei I phase, II phase,
to antigens S. flexneri I–VI+ S. sonnei– polyvalent.
To quickly identify Shigella, the following method is recommended: a suspicious colony (lactose-negative on Endo medium) is subcultured on TSI medium (English. triple sugar iron) – three-sugar agar (glucose, lactose, sucrose) with iron to determine H2S production; or to a medium containing glucose, lactose, sucrose, iron and urea. Any organism that breaks down urea after 4 to 6 hours of incubation is most likely a member of the genus Proteus and may be excluded. A microorganism that produces H2S or has a urease or acid-forming joint (fermentes lactose or sucrose) can be excluded, although H2S-producing strains should be investigated as possible members of the genus Salmonella. In all other cases, the culture grown on these media should be examined and, if it ferments glucose (change in the color of the column), isolated in its pure form. At the same time, it can be studied in a glass agglutination reaction with appropriate antisera to the genus Shigella. If necessary, other biochemical tests are performed to check genus membership. Shigella, and also study mobility.
To detect antigens in the blood (including as part of the CEC), urine and feces, the following methods can be used: RPGA, RSK, coagglutination reaction (in urine and feces), IFM, RAGA (in blood serum). These methods are highly effective, specific and suitable for early diagnosis.
For serological diagnosis, the following can be used: RPHA with the corresponding erythrocyte diagnostics, immunofluorescence method (indirect modification), Coombs method (determining the titer of incomplete antibodies). An allergy test with dysenterine (a solution of protein fractions of Shigella Flexner and Sonne) is also of diagnostic value. The reaction is taken into account after 24 hours. It is considered positive in the presence of hyperemia and infiltrate with a diameter of 10–20 mm.
Treatment. The main attention is paid to restoring normal water-salt metabolism, rational nutrition, detoxification, rational antibiotic therapy (taking into account the sensitivity of the pathogen to antibiotics). A good effect is achieved by early use of a polyvalent dysentery bacteriophage, especially tablets with a pectin coating, which protects the phage from the action of gastric juice HCl; In the small intestine, pectin dissolves, phages are released and exert their effect. For preventive purposes, the phage should be given at least once every three days (the period of its survival in the intestine).
The problem of specific prevention. To create artificial immunity against dysentery, various vaccines were used: from killed bacteria, chemical, alcohol, but all of them turned out to be ineffective and were discontinued. Vaccines against Flexner's dysentery have been created from live (mutant, streptomycin-dependent) Shigella Flexner; ribosomal vaccines, but they also have not found widespread use. Therefore, the problem of specific prevention of dysentery remains unresolved. The main way to combat dysentery is to improve the water supply and sewerage system, ensure strict sanitary and hygienic regimes in food enterprises, especially the dairy industry, in child care institutions, public places and in maintaining personal hygiene.
Lecture No. 7. ^ Escherichia and Shigella .
Genus Escherichia.
Escherichia is the most common aerobic intestinal bacteria that, under certain conditions, can cause a wide group of human diseases, both intestinal (diarrhea) and extraintestinal (bacteremia, urinary tract infections, etc.) localization. The main species is E. coli (Escherichia coli) - the most common causative agent of infectious diseases caused by enterobacteria. This pathogen is an indicator of fecal contamination, especially in water. If - titer and if - index were often used as sanitary indicators. Escherichia is part of the microflora of the large intestine of mammals, birds, reptiles and fish.
^ Cultural properties. On liquid media, E. coli produces diffuse turbidity; on solid media, it forms S- and R-form colonies. On Endo, the main medium for Escherichia, lactose-fermenting E. coli form intensely red colonies with a metallic sheen; non-fermenting ones form pale pink or colorless colonies with a darker center; on Ploskirev’s medium they are red with a yellowish tint; on Levin’s medium they are dark blue with a metallic sheen. .
^ Biochemical properties. In most cases, E. coli ferments carbohydrates (glucose, lactose, mannitol, arabinose, galactose, etc.) with the formation of acid and gas, produces indole, but does not form hydrogen sulfide, and does not liquefy gelatin.
^ Antigenic structure. No significant morphological differences were found between pathogenic and non-pathogenic Escherichia coli. Their differentiation is based on the study of antigenic properties. Among the surface antigens, polysaccharide O-antigens, flagellar H-antigens and capsular polysaccharide K-antigens are distinguished. More than 170 variants of O-antigens are known (this corresponds to the pathogen belonging to a certain serogroup) and 57 - H-antigens (belonging to serovar). Part diarrheagenic(diarrhea-causing) Escherichia coli includes 43 O-groups and 57 OH-variants.
^ The main pathogenicity factors of diarrheagenic E.coli.
1. Factors of adhesion, colonization and invasion associated with pili, fimbrial structures, and outer membrane proteins. They are encoded by plasmid genes and promote colonization of the lower small intestine.
2. Exotoxins: cytotonins (stimulate hypersecretion of fluid by intestinal cells, disrupt water-salt metabolism and promote the development of diarrhea) and enterocytotoxins (act on the cells of the intestinal wall and capillary endothelium).
3. Endotoxin (lipopolysaccharide).
Depending on the presence of various pathogenicity factors, diarrheagenic E. coli are divided into five main types: enterotoxigenic, enteroinvasive, enteropathogenic, enterohemorrhagic, enteroadhesive.
4. Pathogenic E. coli are characterized by the production of bacteriocins (colicins).
EnterotoxigenicE. coli have a high-molecular heat-labile toxin, similar in action to cholera, causing cholera-like diarrhea (gastroenteritis in young children, travelers' diarrhea, etc.).
^ Enteroinvasive Escherichia coli able to penetrate and multiply in intestinal epithelial cells. They cause profuse diarrhea mixed with blood and a large number of leukocytes (an indicator of an invasive process) in the feces. Clinically resembles dysentery. The strains have some similarities with Shigella (stationary, do not ferment lactose, and have high enteroinvasive properties).
EnteropathogenicE. coli - the main causative agents of diarrhea in children. The lesions are based on the adhesion of bacteria to the intestinal epithelium with damage to microvilli. Characterized by watery diarrhea and severe dehydration.
^ Enterohemorrhagic Escherichia coli cause diarrhea mixed with blood (hemorrhagic colitis), hemolytic-uremic syndrome (hemolytic anemia in combination with renal failure). The most common serotype of enterohemorrhagic Escherichia coli is O157:H7.
EnteroadhesiveE. coli do not form cytotoxins, poorly studied.
Epidemiology. The main mechanism of spread of diarrheagenic E. coli is fecal-oral. Infection can occur through food, water, and when caring for animals. Since Escherichia live in the intestines of many animal species, it is difficult to determine the specific source of infection. The contact route of infection can be in closed establishments. Enteropathogenic and enteroinvasive E. coli are the most common causes of nosocomial outbreaks of escherichiosis.
^ Laboratory diagnostics. The main approach is the isolation of a pure culture on differential diagnostic media and its identification by antigenic properties. RA is placed with a set of polyvalent OK (to O- and K-antigens) sera, then adsorbed O-sera and cultures heated at 100 degrees Celsius (to destroy K-antigens).
Biochemical differentiation is of additional importance. Identification of diarrheagenic types is possible by identifying specific markers (enterohemorrhagic E. coli do not ferment sorbitol, and serovar O157:H7 does not exhibit beta-glucuronidase activity).
Genus Shigella.
Shigella is an intestinal pathogen of humans and primates that causes bacillary dysentery or shigellosis. In accordance with the antigenic structure of the O-antigen and biochemical properties, the known serotypes of Shigella are divided into four species or serogroups - S.dysenteriae (serogroup A), S.flexneri (serogroup B), S.boydii (serogroup C) and S.sonnei (serogroup D).
By morphological characteristics Shigella is no different from other enterobacteria. These are non-specific facultative anaerobic gram-negative rods.
^ Biochemical properties. Shigella is biochemically inactive compared to other intestinal bacteria. They do not form hydrogen sulfide on three-sugar iron agar and do not ferment urea.
Strains of S.dysenteriae (serogroup A) have the least enzymatic activity, fermenting only glucose without gas formation; unlike other Shigella, this species is mannitol-negative.
Shigella Flexner ferment mannitol and form indole, but do not ferment lactose, dulcit and xylose. The Newcastle serotype is divided into three biochemical types. For Shigella Flexner, the waterborne route of transmission is more typical.
Boyd's Shigella (serogroup C) have similar biochemical activity, but ferment dulcite, xylose and arabinose. They have a number of serotypes, each of which has its own main type antigen.
Shigella Sonne (serogroup D) is capable of slowly fermenting lactose and sucrose and has biochemical types and phagotypes. The main route of transmission is food (usually through milk and dairy products).
^ Antigenic structure. Shigella has O- and K-antigens. O-antigens have epitopes of varying specificity - from those common to the family of enterobacteria to type-specific ones. The classification takes into account only thermostable group (four groups or types - A, B, C and D) and type-specific (division into serotypes). Heat-labile antigens include K-antigens (they are found in groups A and C) and fimbrial antigens (in Shigella Flexner they are antigenically similar to E.coli). Determination of the antigenic structure is necessary for final identification.
Epidemiology. Shigella is quite stable in the external environment. The source of infection is a person with various forms of clinical manifestations of shigellosis. The mechanism of infection is fecal-oral. Different types of Shigella are characterized by the predominant routes of transmission (contact-household - for S.dysenteriae, food - for S.sonnei, water - for S.flexneri). The epidemic process is characterized by a change in the structure of circulating populations of pathogens - a change in leading species, biovars, serovars, which is associated both with changes in population immunity and with changes in the properties of the pathogen, especially with the acquisition of various plasmids (R, F, Col, etc.). The infectious dose is about 200 - 300 Shigella. Dysentery caused by Shigella Sonne has a milder course.
^ Pathogenicity factors and pathogenesis of lesions. The main biological characteristic of Shigella is the ability to invade epithelial cells, multiply in them and cause their death. The formation of a lesion in the mucosa of the descending colon (sigmoid and rectum) is cyclical: adhesion, colonization, introduction of Shigella into the cytoplasm of enterocytes, reproduction, destruction and rejection of epithelial cells, release of Shigella into the intestinal lumen, adhesion again, etc.
Role adhesion and colonization factors performed by pili, outer membrane proteins, LPS, enzymes - neuraminidase, mucinase, hyaluronidase (destroy mucus).
Shigella has a range of factors of invasion and resistance to the action of defense mechanisms (K-antigen, LPS, etc.) controlled by Shigella chromosomal genes and plasmids.
Shigella have different toxins. They have endotoxin and Shiga-like cytotoxins (SLT-1, SLT-2). Cytotoxins cause cell destruction, enterotoxin causes diarrhea, and endotoxin causes general intoxication. Shiga Toxin causes disruption of protein synthesis, absorption of sodium and water ions, and fluid influx into the site of inflammation.
The most typical signs of dysentery are diarrhea, tenesmus(painful spasms of the rectum) and frequent urges, general intoxication. The nature of the stool is determined by the degree of damage to the large intestine.
^ Post-infectious immunity - durable, type-specific.
Laboratory diagnostics. The main diagnostic method is bacteriological. The feces are inoculated on the differential diagnostic media Endo and Ploskirev to obtain isolated colonies. Pure cultures are studied according to their biochemical properties, identification is carried out in RA with poly- and monovalent sera. If the isolated culture has the biochemical properties of Shigella, but does not agglutinate sera to O-antigens, it must be boiled for 30 minutes to destroy heat-labile K-antigens, which often prevent the agglutination of Shigella serogroups A and C (i.e., having K-antigens), and again research in RA.
For serological diagnosis, RPGA with group erythrocyte diagnostics is used.
^
Lecture No. 8. Representatives of the generaVibrio,
Campylobacter,
Helicobacter.
Genus Vibrio.
The Vibrionaceae family includes motile, curved, rod-shaped bacteria with polar flagella. Evolutionarily originated from aquatic bacteria, they are widely distributed in fresh and sea water, in invertebrate and vertebrate hosts. Species pathogenic to humans are classified as genera Vibrio, Aeromonas And Plesiomonas.
The genus Vibrio is characterized by short, straight or curved gram-negative rods, motile, not forming spores or capsules, and growing well on ordinary media. They ferment carbohydrates with the formation of acid without gas, and are sensitive to vibriostatic agent O/129. Can be cultivated at temperatures from plus 18 to 37 o C, pH 8.6-9.0.
Representatives of the genus Vibrio are differentiated from other genera of the family by biochemical tests. The genus contains more than 25 species, of which the main significance is Vibrio cholerae- the causative agent of cholera, as well as V.parahaemolyticum, V.vulnificus.
Vibrio cholerae.
Morphology. Vibrio cholerae has one polar flagellum, often resembling a comma ( Koch comma). An important diagnostic sign is mobility (determined by microscopy using the hanging or crushed drop method). Morphologically variable. They stain well with Pffeffer's water fuchsin and Ziehl's carbolic fuchsin.
^ Cultural properties. Facultative anaerobe. Vibrio cholerae is unpretentious to nutrient media. It multiplies well in 1% alkaline (pH 8.6-9.0) peptone water, outstripping bacteria of the intestinal group (enrichment medium), and forms a delicate bluish film and turbidity. To suppress the growth of Proteus and some other microorganisms, peptone water with the addition of potassium tellurite is used.
On dense media, Vibrio cholerae forms smooth, glassy, transparent disc-shaped colonies with a bluish tint of viscous consistency. Use alkaline agar, bile salt agar, alkaline blood agar, the best is TCBS agar (agar with thiosulfate, citrate, bile salts and sucrose).
^ Biochemical properties. Vibrio cholerae ferments many carbohydrates (glucose, sucrose, mannose, mannitol, lactose, levulose, glycogen, starch) with the formation of acid without gas. In relation to three sugars ( Heiberg's triad) - sucrose, mannose and arabinose, vibrios are divided into eight biochemical groups, Vibrio cholerae belongs to the first group (decomposes sucrose and mannose).
Vibrio cholerae decomposes gelatin, casein, coagulates milk and decomposes protein preparations into indole and ammonia.
The species V.cholerae is divided into biotypes, serogroups And serovars.. The main biotypes are classic (V.cholerae asiaticae) and El Tor (V.cholerae eltor). Serogroups are distinguished by the structure of O-antigens; in the main O1 group of Vibrio cholerae, serovars Ogawa, Inaba and Hikojima are distinguished.
^ Antigenic structure. In Vibrio cholerae, thermostable O-antigens and thermolabile H-antigens are isolated. Based on the structure of O-antigens, 139 serogroups have been identified, the El Tor and classic biotypes are combined into 01 group (typed by 01 antiserum). El Tor isolates are distinguished by hemolytic properties (cause hemolysis of sheep erythrocytes), the ability to agglutinate chicken erythrocytes, resistance to polymyxin, and sensitivity to phages.
O-antigen of group 01 is heterogeneous and includes a common A-component and two type-specific ones - B and C. According to their presence, serovar Ogawa has the combination AB, Inaba - AC, Hikojima - ABC.
Vibrio cholerae can pass from the S- to the R- form without being agglutinated by the O- serum. Due to the antigenic structure, O-serum, OR-serum (to identify OR- and R-dissociates), type-specific sera Inaba (C) and Ogawa (B) are used to identify V.cholerae. In the 90s, a new serovar V.cholerae 0139 was identified, which is not agglutinated by the above sera, and in other properties differs little from Vibrio cholerae group 01.
Vibrios not typed by the main 01 serum (i.e., not belonging to group 01) are called non-agglutinating (NAG) vibrios - cholera-like or paracholera. They have an H-antigen in common with Vibrio cholerae, but differ in the O-antigen.
Based on the H-antigen, groups A and B are distinguished; cholera vibrios are included in group A. Group B virions (biochemically different from cholera vibrios) have a heterogeneous structure of the O-antigen and are divided into six serological subgroups.
^ Pathogenicity factors of Vibrio cholerae.
1. Mobility(flagella) and chemotaxis.
2. Enzymes promote adhesion and colonization, interaction with epithelial cells - mucinase (thin the mucus), neutaminidase (interaction with microvilli, creation of a landing site), lecithinase and others.
3. Endotoxin- thermostable lipopolysaccharide, similar in structure and properties to other endotoxins of gram-negative bacteria.
4. Exotoxin - cholerogens- the main pathogenicity factor, a heat-labile protein. Cholerogen synthesis is the most important, genetically determined property of Vibrio cholerae. The cholerogen molecule consists of two fragments A and B. The actual toxic function is performed by peptide A 1 of fragment A. The cholerogen molecule recognizes the enterocyte receptor, penetrates the cell membrane, activates the adenylate cyclase system, the accumulating cyclic AMP causes hypersecretion of fluid, Na +, HCO 3 -, K + , Cl - from enterocytes. This leads to diarrhea, dehydration and desalination of the body, characteristic of cholera.
5. In many vibrios, incl. not belonging to group 01, there are various enterotoxins.
6. In the pathogenesis of cholera manifestations, a factor that increases capillary permeability is also important.
^ Some features of epidemiology. Cholera is an intestinal infection. The main source is a person (sick or vibration carrier), contaminated water. The method of infection is fecal-oral. Individual susceptibility to cholera is extremely variable. Characterized by a large number of hidden (erased) forms, vibriocarriage. The detection of a pathogen in water is directly related to the presence of patients or bacteria carriers. Cholera vibrios of group 01 can remain in aquatic ecosystems for a long time in the form uncultivated forms.
^ Laboratory diagnostics. Cholera belongs to the group of especially dangerous infections; the cultivation of its causative agent requires compliance with a special biological safety regime. The main diagnostic method is bacteriological, which includes isolation and identification of the pathogen.
Material for research - feces and vomit, sectional materials from the dead, water samples and swabs from environmental objects, food remains.
For inoculation, liquid enrichment media, alkaline MPA, selective and differential diagnostic media (preferably TCBS) are used. 1% peptone water is most convenient as a transport medium. Suspicious glassy transparent colonies are subcultured to obtain a pure culture, which is identified by morphological, cultural, biochemical properties, motility, antigenic properties, and phagotyped.
For accelerated diagnostics, the immunoluminescent method, biochemical identification with a set of indicator disks are used, for the detection of vibrios cholera in primary materials - RNGA with an antibody diagnosticum, for the detection of uncultivable forms - PCR, for the determination of virulence and choleragen synthesis - bioassays on suckling rabbits, ELISA, DNA - probes (detection of a chromosome fragment carrying a cholerogen operon).
^ Specific prevention. There are various vaccines - killed from the serovars Inaba and Ogawa, choleragen toxoid, chemical bivalent vaccine. Vaccines are used only for epidemiological indications (low immunogenicity). Antibiotic prophylaxis (preventive therapy) with tetracycline and other antibiotics can be carried out.
V. parahaemolyticus(parahemolytic vibrio) is a halophile, found in sea water (Japanese, Black, Caspian and other southern seas). When consuming seafood products that have not been subjected to sufficient heat treatment, this pathogen causes foodborne illnesses and dysentery - similar diseases - in people. Causes hemolysis on blood agar with an increased concentration of sodium chloride (7% NaCl - strains with enteropathogenic properties).
V.
vulnificus- the most pathogenic species of non-cholera vibrios for humans. Detected in sea water and its inhabitants. Causes wound infections, septicemia and other diseases. It ferments sucrose and lactose and forms yellow colonies on TCBS agar.
^
Representatives of the genera Campylobacter and Helicobacter.
The gram-negative microaerophiles of these two genera are small, motile, non-spore-forming, curved (S-shaped or gull-wing-like) rod-shaped bacteria. Species that make up the genus Helicobacter, including H. pylori, the causative agent of human peptic ulcer disease, are isolated from the genus Campylobacter.
^ Genus Campylobacter
This genus includes 13 species of spiral bacteria with one or more curls. Campylobacters are motile microorganisms with polar flagella (or flagellum) and helical movement. They do not ferment or oxidize carbohydrates, caprophyles and microaerophiles, i.e. require an increased concentration of CO 2 and a decreased concentration of O 2 .
The genus includes species pathogenic to humans and warm-blooded animals. The diseases they cause are campylobacteriosis - acute intestinal diseases that occur with damage to the gastrointestinal tract. Campylobacters are often isolated from the intestines, oral cavity, and genitourinary organs of warm-blooded animals.
There is a group of C.jejuni (includes this species, as well as C.coli, C.lari) or thermophilic campylobacteria. They are distinguished by a high temperature optimum for growth (+42 0 C).
Among the mesophilic campylobacteria with optimal growth at +37 0 C, C.fetus plays a significant role in human pathology (causes arthritis, meningitis, vasculitis, abortion), and there are also a number of conditionally pathogenic species (C.concisus and C.sputorum - in the oral cavities, C.fennelliae, C.cinaedi and C.hyointestinalis - in the large intestine).
^ Cultural properties. Campylobacters require special gas mixtures to create microaerophilic conditions, pH - 7.0-7.2, mesophilic conditions (+42 0 C for thermophiles, +37 0 C for others). They use special nutrient media (meat, liver, blood) with the addition of selective antibiotics. To obtain purer samples for culture (coprofiltrates are often studied!), filtration through membrane filters with a pore diameter of 0.65 µm can be used. On dense media they form two types of colonies - “spreading” with uneven edges or shiny convex ones with smooth edges, small colonies.
^ Biochemical properties. They are inert to carbohydrates, reduce nitrates, oxidase are positive, energy is obtained from amino acids and tricarboxylic acids. Differentiation of species by biochemical properties is based on hydrolysis of hippurate(C.jejuni and C.coli), sensitivity to nalidixic acid(C.jejuni and C.lari), formation of hydrogen sulfide, etc.
^ Antigenic structure. Campylobacters have O-, H- and K-antigens. Thermally stable O-antigens are of primary importance for serotyping.
Epidemiological features. Campylobacter is common in various species of mammals and birds. The main route of transmission is food. Predominantly summer seasonality is typical.
^ Main pathogenetic factors. Campylobacters are characterized by high adhesive and invasive activity, rapid colonization of the upper parts of the small intestine. The most important adhesion factors are flagella and specific surface adhesins. These bacteria have endotoxin, a heat-labile enterotoxin.
^ Clinical manifestations - enterocolitis.
Laboratory diagnostics. Microscopic method - staining with a 1% aqueous solution of basic fuchsin for 10-20 seconds - reveals S-shaped short chains, “gull wings”. The main method is bacteriological - stool culture. Cultures are identified by a set of characteristics.
^ Helicobacter pylori.
Peptic ulcer is a disease that is characterized by the presence of an ulcerative defect in the gastric mucosa or duodenum. The discovery of H. pylori led to a revolution in ideas about the etiology, pathogenesis, treatment and prevention of peptic ulcer disease. Peptic ulcer disease is almost 100% associated with Helicobacter pylori. Stress factors and psychological characteristics of patients, as well as genetic factors in the development of the disease also play a significant role.
^ Morphological and cultural properties - similar to Campylobacter. Prefers chocolate agar.
Biochemical properties. Has urease, oxidase- and catalase-positive.
^ Antigenic properties. Has O- and H-antigens.
Pathogenesis of lesions. Helicobacter penetrates through the mucus layer (usually in the antrum of the stomach and duodenum), attaches to epithelial cells, and penetrates the crypts and glands of the mucous membrane. Bacterial antigens (primarily LPS) stimulate neutrophil migration and cause acute inflammation. Helicobacter are localized in the area of intercellular passages, which is due to chemotaxis to urea and hemin (destruction of erythrocyte hemoglobin in the microvasculature). Under the influence of Helicobacter urease, urea is broken down into ammonia, the action of which is associated with damage to the mucous membrane of the stomach and duodenum. Many enzymes (mucinase, phospholipase, etc.) can also stimulate disruption of the integrity of the mucous membranes.
The pathogenicity factors of H. pylori primarily include colonization factors (adhesion, motility), persistence factors and disease-causing factors. Key factors in the tropism and pathogenicity of H. pylori include mechanisms of adhesion and secretion of bacterial toxins. Evidence is presented for the leading role of Lewis B antigen as an adhesion receptor. In addition to them, gastric mucins and sulfatides of the gastric mucosa are important. The pathogen's Bab A protein (adhesin) has been identified, which allows the microorganism to bind to the Lewis B blood group antigen present on the surface of gastric epithelial cells. Other pathogenicity factors include cag A (cytotoxin-associated gene) and vac A (vacuolating cytotoxin). Strains expressing these virulence markers belong to the first type strains, which are associated with increased ulcerogenic and inflammatory potential, in contrast to the second type strains, which do not have these factors.
The presence of all three factors (Bab A, cag A, vacA) is essential for the manifestation of the pathogenic properties of H. pylori (triplet - positive strains). The damaging effect on the mucosa can be associated both with the direct effect of bacterial toxins, and with indirect effects through the immune system. Long-term persistence of the pathogen is associated with a number of mechanisms that allow it to overcome the protective barriers of the mucous membrane, and the ability to form coccal forms that do not have pathogenic potential.
H. pylori does not always lead to the development of peptic ulcers, but in peptic ulcers this pathogen is constantly detected. Factors that determine the ulcerogenicity of H. pylori are being intensively studied.
^ Laboratory diagnostics should be comprehensive, based on several tests. Detection methods can be invasive (associated with the need to take a biopsy of the mucous membrane) and non-invasive (indirect).
^ Basic methods for detecting H. pylori in mucosal biopsies.
1.Microscopic methods (staining with hematoxylin-eosin, acridine orange, Gram, water fuchsin, silver inpregnation; phase-contrast microscopy with determination of mobility).
2. Determination of urease activity.
3. Isolation and identification of the pathogen on solid media (usually blood). Cultures are carried out on blood agar, blood agar with amphotericin, erythritol - agar with amphotericin. Cultivate for 5-7 days at 37 o C in microaerophilic, aerobic and anaerobic conditions. Affiliation is determined by the morphology of microorganisms and their colonies, helical mobility, growth in microaerophilic conditions and the absence of growth in aerobic and anaerobic conditions and at temperatures of +25 and +42 o C, by the presence of oxidase, catalase and urease activity.
4. Detection of pathogen antigens in ELISA.
5.PCR diagnostics is the most sensitive and specific test.
Non-invasive methods include a “breath test” and ELISA to detect IgG and IgA antibodies.
Treatment complex, using sanitation methods (causative agent radiation). De-NOL (colloidal bismuth subcitrate), ampicillin, trichopolum (metronidazole), etc. are used.
Dysentery is one of those few infectious diseases that have not only been known to mankind since antiquity, but also still retain their original name. Hippocrates used the term “dysentery” to describe a clinical syndrome characterized by diarrhea and abdominal pain. It is quite natural that completely different diseases were hidden under this definition. The term closest to the modern definition of dysentery is sekiri (“red diarrhea”), which was common in China and Japan and was used to describe diseases characterized by loose stool mixed with mucus, blood, and pain during bowel movements.
In 1875, the Russian doctor F.A. Lesh managed for the first time to detect amoebas in the stool of patients with dysentery. It was surprising that, despite frequent epidemics of dysentery at the end of the 19th century, it was not possible to identify amoebas in the stool of patients either in Europe or in Japan. Although the bacterial etiology of dysentery was assumed in these cases, no one was able to diagnose it for a long time. Only in 1898, the Japanese researcher Kiyoshi Shiga isolated a bacillus from the feces of patients, which was recognized as the causative agent of bacterial dysentery. Due to the establishment of different etiologies of dysentery, in the first half of the twentieth century the terms “bacillary” and “amoebic” dysentery were used in the medical literature. Currently, dysentery refers only to diseases caused by Shigella.
In terms of prevalence, acute intestinal infections (AI) are second only to respiratory viral diseases. Recent decades have been marked by certain advances in the study of the etiopathogenesis of acute intestinal infections. If before 1970, only 10% of hospitalized patients had an established etiology of the disease, then by the end of the twentieth century this figure increased to 50-60%. Despite the identification of new pathogens of acute intestinal infections, shigellosis continues to occupy a significant position in the etiological structure of acute infectious diarrheal diseases. According to the Federal Center for State Sanitary and Epidemiological Surveillance, in Russia in 2002, 80,500 cases of dysentery were registered (incidence rate 55.96 per 100 thousand population), of which children under 14 years old accounted for 38,5000 (incidence rate 159.1 per 100 thousand). ). In the USA, according to the National Committee for Infectious Disease Control (CDC), from 25 to 30 thousand cases of shigellosis are registered annually with an incidence rate for children from one to four years old - 27 per 100 thousand population, and for persons over 20 years of age - 2.6 per 100 thousand.
Etiology. Since 1930, bacilli isolated from dysentery patients were officially united into the genus Shigella, family Enterobacteriaceae. Shigella are identified by their biochemical and antigenic properties (O - antigens), according to which four groups of Shigella are distinguished (see Table 1).
Shigella is relatively resistant to environmental factors and can survive on household items for a long time; in water they remain viable for up to two to three weeks, and in a dried and frozen state for up to several months. High temperatures, on the contrary, contribute to their rapid death: at a temperature of +60°C - within 10 minutes, and when boiling - instantly. Shigella exhibits fairly high sensitivity to disinfectants, ultraviolet and direct sunlight.
Epidemiology. Shigellosis refers to classic anthroponotic intestinal infections, which are characterized by a fecal-oral transmission mechanism of infection, realized by all possible routes for this mechanism - food, water and contact. However, the practical implementation of each of these transmission routes depends on many factors and conditions (type of Shigella, age of the patient, his premorbid background, etc.). Since they have the greatest virulence Sh. dysenteriae 1, it is for them that the contact route of transmission of infection is most characteristic, although this route can also be realized by other types of Shigella, especially in young children, elderly and weakened patients. Numerous observations indicate that in case of group cases of diseases, certain types of Shigella have their own, most typical route of infection transmission (contact for group A, food for group D and water for groups B and C). In recent years, sexual transmission of shigella infection among homosexuals has been described (1). In particular, during an outbreak of shigellosis caused by Sh. sonnei(biotype G), in one of the clubs in New South Wales (Australia) between January 1 and July 31, 2000, 148 cases were registered, 80% of whom were homosexuals.
Despite the diversity of shigellosis pathogens, the greatest epidemic significance for most countries of the world are Sh. flexneri And Sh. sonnei. Although Shigella is widespread (an anthroponotic infection), the highest incidence rates are recorded in countries and regions with poor sanitation and high population density, which greatly facilitates the possibility of transmission of the pathogen from person to person. According to estimates, about 140 million cases of shigellosis are registered annually in the world. Susceptibility to shigella infection varies among individuals of different age groups. Children under two or three years of age are most susceptible to them.
Pathogenesis. The basis of the pathogenesis of infectious diseases is the characteristics and nature of the interaction of microbes not only with the cells of the macroorganism, but also with the nonspecific and specific defense systems of the body.
Shigella has quite pronounced virulent properties, as a result of which the disease can develop even with a low infectious dose (in comparison with enteropathogenic bacteria such as salmonella and E. coli). Due to the relative resistance to the action of gastric juice and bile acids, Shigella, without losing its virulence, passes through the gastric barrier and the proximal parts of the small intestine. In the pathogenesis of the disease, small and large intestinal phases are distinguished, the severity of which ultimately determines the course of the disease. In patients with the typical, colitic variant of acute dysentery, the small intestinal phase is not clinically manifested at all, and the disease initially manifests itself as damage to the distal colon. The small intestinal phase is usually short-lived and limited to two to three days. The primary translocation of Shigella through the epithelial barrier is carried out by specialized M cells capable of transporting both the bacteria themselves and their antigens into the intestinal lymphatic formations (follicles, Peyer's patches) with their subsequent penetration into epithelial cells and resident macrophages. Toxic substances released during the translocation of Shigella (exo- and endotoxins, enterotoxins, etc.) initiate the development of intoxication syndrome, which in shigellosis always precedes the development of diarrhea syndrome.
Intestinal motility is an important protective mechanism that limits and prevents the attachment and invasion of Shigella to epithelial cells, which is clearly demonstrated by the prolongation and severity of the infectious process in individuals receiving drugs that suppress intestinal motility.
The dysbiotic changes in the composition of the normal microflora of the large intestine observed in patients with shigellosis have a significant impact on the rate of mucosal repair in the convalescence stage and restoration of the functional activity of the intestine.
After suffering from the disease, patients develop short-term (up to one year) type- and species-specific immunity, due to which reinfection is possible.
Clinic. The clinical picture of shigellosis is very variable, which is reflected in the applied clinical classification of the disease (see Table 2). Although it is believed that Sh. sonnei, Since less virulent strains of Shigella often cause milder forms of the disease, it should be remembered that the etiology of shigellosis only predetermines, but does not determine the characteristics of the course of the disease in specific patients (in terms of form, variant and severity).
The chronic form of dysentery is currently quite rare and, according to the literature, does not exceed 1-2% of cases, although there is an opinion that such a low proportion of it may be due to insufficiently developed diagnostic criteria. Much more often, doctors in their practice encounter acute forms of shigellosis, which are of the greatest interest in terms of an adequate assessment of the clinical picture of the disease detected in the patient, the completeness of the examination, the correctness and timeliness of the therapy.
The incubation period for shigellosis can vary from 8-12 hours (with the gastroenteric variant) to five days (with the colitis variant of the disease), averaging two to three days.
A typical course of acute dysentery is colitis, its characteristic feature is the acute onset of the disease with the development of an intoxication syndrome: a rise in body temperature, chills, fever, weakness, a feeling of weakness, headache, and loss of appetite. With this variant of acute dysentery, intoxication syndrome always precedes clinical manifestations of intestinal damage. Only after some time (from 2-3 to 12-18 hours) do patients show signs of damage to the gastrointestinal tract. Initially, patients note the occurrence of diffuse, dull pain, which over time becomes more acute and acquires a cramping character. The localization of pain most often corresponds to the projection area of the distal colon (lower abdomen and left iliac region). Almost simultaneously with abdominal pain, patients note the appearance of diarrhea. For the colitic variant of dysentery, the relationship between the development of an attack of abdominal pain and defecation, the urge to which appears at the height of a painful attack, is typical. Since abdominal pain is caused by spastic contraction of the intestine (increased intestinal motility), the first bowel movements are relatively abundant, but quite quickly they decrease in volume (“scanty stool”), lose their fecal character, and pathological impurities appear in them - mucus and blood. As a rule, bowel movements occur more than five times a day (often up to 15-20 or more). Quite often, patients experience tenesmus, and in more severe cases, false urges. An objective examination of patients reveals a painful and spasmodic sigmoid colon.
If mucus in the stool is a typical sign of acute dysentery, then blood may be present in microscopic quantities and can only be detected during coprocytoscopic examination. Visualized blood in the stool is determined in the form of streaks. In more severe cases of the disease, defecation may result in the release of a small amount of mucus streaked with blood.
Criteria for the severity of the course of the colitic variant of acute dysentery are the severity of the intoxication syndrome and the nature of the damage to the distal mucosa of the large intestine (see Table 3). Severe dehydration in patients with the colitic variant of acute dysentery is not detected due to the absence of vomiting and scanty stool.
The gastroenterocolitic variant of dysentery is also characterized by an acute onset of the disease: with chills, fever, headache and the simultaneous appearance of gastroenteritis syndrome - spastic pain in the epigastric region, nausea, vomiting, loose watery stools. Clinical signs of colitis are usually absent on the first day of the disease and appear only after one to three days, which corresponds to the pathomorphological stages of damage to the gastrointestinal mucosa. Depending on the frequency of vomiting and the intensity of diarrhea syndrome, patients show signs of dehydration quite early (dry mucous membranes of the oropharynx, pale skin and cyanosis, pointed facial features, decreased blood pressure, oliguria, etc.). From the moment the pathological process spreads to the mucous membrane of the large intestine, the manifestations of gastroenteritis gradually stop: vomiting stops, the volume of bowel movements decreases, and pathological impurities (mucus and blood) appear in the stool. Depending on the nature of the damage to the mucous membrane of the distal colon, patients may notice the appearance of tenesmus and false urges. When palpating the abdomen in the first days of the disease, rumbling along the course of the large intestine is noted, and in subsequent days pain and spasm of the sigmoid colon appears and increases.
The severity of the gastroenterocolitic variant of dysentery is determined based on the severity of intoxication and dehydration of the body. In most cases it does not exceed grades II-III.
A rare variant of the course of acute dysentery is gastroenteric, characterized by great similarity with foodborne toxic infections.
Complications. Although the risk of complications is highest in patients with dysentery caused by Sh. dysenteriae 1, At the present stage, there is a clear tendency towards an increase in severe forms of dysentery caused by other types of Shigella (in particular, Sh. flexneri), which, accordingly, affects the possibility of developing complications. The most dangerous complications include: infectious-toxic shock; intestinal perforation with the development of peritonitis; encephalic syndrome (fatal encephalopathy syndrome or Ekiri), which predominantly develops in children and immunocompromised patients with dysentery caused by Sh. sonnei or Sh. flexneri; bacteremia detected in dysentery Sh. dysenteriae 1 in 8% of cases and extremely rarely - when infected with other types of Shigella (in children under one year old, weakened, exhausted and immunocompromised patients); hemolytic-uremic syndrome, developing a week from the onset of the disease and characterized by microangiopathic hemolytic anemia, thrombocytopenia and acute renal failure. Often, patients may develop complications associated with the activation of secondary microflora: pneumonia, otitis, urinary tract infections, etc. Rare but probable complications include reactive arthritis and Reiter's syndrome (about 2% of patients expressing HLA-B27). In recent years, the possible role of shigellosis in the formation of irritable bowel syndrome has been discussed.
Diagnosis and differential diagnosis. Specific diagnosis of shigellosis is based on the isolation and identification of Shigella from the patient's feces and conducting serological and/or immunological studies aimed at detecting Shigella antigens or antibodies to them. Without laboratory confirmation, the diagnosis of dysentery can only be established with a typical clinical picture.
Although the diagnostic value of endoscopic examination of the colon (sigmoidoscopy and fibrocolonoscopy) in patients with suspected shigellosis is limited, the information obtained during its implementation allows: a) to objectively assess the nature of the damage to the colon mucosa; b) carry out differential diagnosis and c) monitor the effectiveness of the therapy.
Depending on the nature of the lesion, the following variants of proctosigmoiditis are distinguished: catarrhal, catarrhal-hemorrhagic, erosive, erosive-ulcerative and fibrinous, which, as a rule, correspond to the severity of the disease.
When carrying out differential diagnosis, it is first necessary to exclude other acute intestinal infectious diseases, for which the development of exudative diarrhea is typical, namely enteroinvasive escherichiosis, salmonellosis, yersiniosis ( Y. enterocolitica), campylobacteriosis ( Campylobacter jejuni), infection Clostridium difficile and amebiasis (protozoal disease caused by Entamoeba histolytica). In addition, it must be remembered that diseases such as ulcerative colitis and Crohn's disease can debut under the guise of shigellosis.
Treatment. Treatment of patients with dysentery can be carried out not only in a specialized infectious diseases department, but also on an outpatient basis, which is determined by clinical and epidemiological indications. First of all, patients with moderate and severe forms of the disease should be hospitalized, with a protracted and chronic course - patients with severe concomitant diseases, children under one year old and the elderly, as well as persons posing an epidemic danger (regardless of the variant and severity of the disease) - workers food enterprises and persons equated to them.
Given the nature of the damage to the intestinal mucosa, patients with dysentery, especially during the acute period of the disease, need strict adherence to therapeutic nutrition. Any foods that have an irritating (mechanical, chemical, etc.) effect should be excluded from the diet. Due to lactose deficiency developing in patients, whole milk is excluded from the diet. The expansion of the diet is carried out gradually, only as the patient recovers. And yet, the transition to normal nutrition should be carried out no earlier than complete recovery, characterized by repair of the mucous membrane (see Table 3).
Since antibacterial therapy has always been recommended for the treatment of patients with dysentery, a serious problem today is the development of resistance to antimicrobial drugs in Shigella, especially in those countries where they are sold over the counter and self-medicated. Recent studies in our country have confirmed the high frequency of resistance in Sh. flexneri And Sh. sonnei to cefotaxime (96.6 and 94.2%, respectively), tetracycline (97.7 and 92.8%), chloramphenicol (93.2 and 50.7%), ampicillin (95.5 and 26.1) and ampicillin/sulbactam (95.5 and 23.2%). Resistance was not detected only to ciprofloxacin, norfloxacin and nalidixic acid.
The choice of an antimicrobial drug and the regimen for its use in patients with dysentery are determined by the type and severity of the disease. With the gastroenteric variant, antimicrobial therapy is not indicated and patients are prescribed only pathogenetic therapy. For mild colitic and gastroenterocolitic variants of dysentery, it is advisable for patients to be prescribed furazolidone 0.1 g four times a day or nalidixic acid (nevigramon) 0.5-1.0 g four times a day for three to five days. The most effective drugs for treating patients with moderate and severe dysentery are fluoroquinolone drugs (ciprofloxacin, norfloxacin, etc.), third generation cephalosporins (cefotaxime), which are prescribed in general therapeutic doses for five to seven days. In severe cases, combined antibacterial therapy (fluoroquinolones and aminoglycosides; cephalosporins and aminoglycosides) can be carried out.
In addition to antibacterial therapy, an important place in the treatment of patients with dysentery is occupied by pathogenetic treatment, including detoxification and rehydration. In the acute period of the disease, it is advisable for patients to be prescribed desmol and smecta, which have an anti-inflammatory and membrane-stabilizing effect on the intestinal mucosa. After relief of the intoxication syndrome, patients are shown drugs that normalize the processes of digestion and absorption (digestal, mezim-forte, panzinorm, festal, cholenzym, oraza, etc.). Correction of intestinal microbiocenosis should be carried out only during the period of convalescence, when the acute inflammatory reaction is stopped. During the same period, patients are shown physiotherapeutic procedures that accelerate the process of repair of the colon mucosa.
Literature
- Centers for Disease Control and Prevention. Shigella sonnei outbreak among men who have sex with men-San Francisco, California, 2000-2001.//MMWR Morb.Mortal.Wkly.Rep.-2002.-v.50.-No. 922.
- Pontivivo G., Karagiannis T., Marriott D. et al. Shigellosis Linked to Sex Venues, Australia.//Emerging Infectious Diseases.- 2002.- v. 8.-No. 8.-r. 862-864.
- Malov V. A., Pak S. G. Medical and biological aspects of the problem of intoxication in infectious pathology // Therapeutic archive. - 1992.- No. 11. - With. 7-11.
- Khalil K., Khan S., Mazhar K et al. Occurrence and susceptibility to antibiotics of Shigella sp. in stool of hospitalized children with bloody diarrhea in Pakistan.//Am.J.Trop.Med.Hyg.-1998.-v.58.-p.800-803.
- Strachunsky L. S., Krechikova O. I., Ivanov A. S. et al. Antimicrobial resistance of Shigella in the Smolensk region in 1998-1999 // Clinical microbiology and antimicrobial therapy. - 2000. - T. 2. - No. 2. - pp. 65-69.
V. A. Malov, Doctor of Medical Sciences, Professor
A. N. Gorobchenko, Candidate of Medical Sciences
MMA im. THEM. Sechenov
Note!
- According to the Federal Center for State Sanitary and Epidemiological Surveillance, in Russia in 2002, 80,500 cases of dysentery were registered (incidence rate 55.96 per 100 thousand population), of which children under 14 years old accounted for 38,5000 (incidence rate 159.1 per 100 thousand). ).
- Despite the identification of new pathogens of acute intestinal infections, shigellosis continues to occupy a significant position in the etiological structure of acute infectious diarrheal diseases.
- Since 1930, bacilli isolated from dysentery patients have been officially grouped into the genus Shigella, family Enterobacteriaceae.
Microbiology: lecture notes Ksenia Viktorovna Tkachenko
3. Shigella
3. Shigella
They belong to the genus Shigella.
They are causative agents of dysentery. The morphology is the same as that of other representatives of the Enterobacteriaceae family. They are immobile and do not form capsules.
They grow well on simple nutrient media. Colorless colonies form on Endo medium.
The genus includes four species that differ in biochemical properties (the ability to ferment mannitol and lactose) and antigenic structure:
1) Sh. disenteriae; do not ferment lactose and mannitol; according to antigenic properties within the species they are divided into 12 serovars; one of them, Shigella Grigorieva-Shiga, is the most pathogenic;
2) Sh. flexneri; ferments only mannitol; according to antigenic properties it is divided into 6 serovars, which are divided into subserovars;
3) Sh. boydii; ferments only mannitol; according to antigenic structure it is divided into 18 serovars;
4) Sh. sonnei; ferments only lactose; Antigenically, the species is homogeneous; within the species, fermentovars, phagovars, and kolecinovars are distinguished.
Shigella, bypassing the stomach and small intestine, enters the large intestine. They attach to colonocyte membrane receptors and penetrate inside using the outer membrane protein. Cell death leads to the formation of erosions and ulcers surrounded by perifocal inflammation.
Pathogenicity factors:
1) proteins of the outer membrane (provide the ability for invasion and intracellular reproduction);
2) contact hemolysin (promotes lysis of cell vacuole membranes);
3) exotoxin (has enterotropic, cyto- and neurotoxic effects);
4) endotoxin (has a general toxic effect on the body and protects Shigella that has entered the body from the action of the protective forces of the macroorganism).
There are three clinical forms of dysentery, which differ in pathogens, epidemiology and partly in clinic:
1) Grigoriev-Shiga dysentery. Pathogen – Sh. disenteriae, serovar – Shigella Grigorieva-Shiga. Routes of transmission: nutritional, contact and household. Features of the clinic: it is severe, characterized by bloody diarrhea with blood, symptoms of central nervous system damage, there may be bacteremia;
2) Flexner's dysentery. Pathogens – Sh. flexneri and Sh. boydii. The route of transmission is water. Features of the clinic: it occurs as typical dysentery of varying severity;
3) Sonnei dysentery. The route of transmission is food. Features of the clinic: there may be symptoms of food poisoning, vomiting.
Diagnostics:
1) bacteriological examination;
2) immunoindication (ELISA);
3) serodiagnosis (has retrospective significance).
Specific prevention: dysentery bacteriophage (used in areas of infection).
Etiotropic therapy: in moderate and severe cases of the disease, antibiotics are prescribed (those that are excreted by the intestines) taking into account the sensitivity of the pathogen.